When a friend or loved one is physically ill or injured, we don’t brand them ‘worthless’ or ‘incompetent’. We don’t tell them “There’s nothing wrong with you”, “it’s all in your head” or “You’re making it up”. Instead, we support them and don’t blink an eye at the thought of them seeing a doctor or specialist for guidance. We help them heal.
But when it comes to mental health and wellbeing there’s still a deeply entrenched stigma within our society. The stigma of mental illness stops us from acknowledging, asking, listening, and supporting someone who is suffering from a mental illness. This is particularly worrying as mental illnesses are not less of a condition than a physical illness or injury. In fact, according to the World Health Organisation (WHO), around 450 million people currently suffer from a mental disorder, which makes mental illness among the leading causes of ill health worldwide.

Mental Health Stigma: Shake it off, shake it off
With one in five Aussies experiencing a mental illness in any given year, it’s no surprise that discourse around mental health conditions has started to become more accepted. Initiatives like ‘R U OK?’ Day and public figures addressing the stigma surrounding mental illness have helped build awareness. However, there’s still a lot of work to be done in uprooting the beliefs about mental illness that stop people from seeking care from counsellors, psychologists and even friends and family.
Stigma is a major cause of discrimination and exclusion. It hampers the promotion of mental well-being and the provision of effective treatment and care. According to a recent German study:
It’s hard enough trying to manage the symptoms associated with different types of mental health conditions, without having to also challenge the stereotypes, discrimination and prejudice surrounding your condition. Understandably, this can make it even more debilitating.
Mental illness refers to a broad range of conditions from depression to anxiety disorders and eating disorders to addiction and personality disorders. It’s not confined to the often sensationalised depictions of people with mental illness in movies and on television.
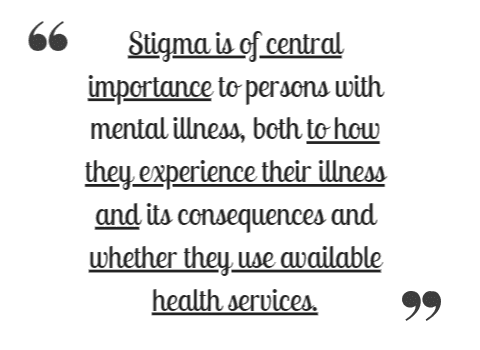
Interestingly, mental illness stigma isn’t just endorsed and cultivated by the public. People affected by mental illness also project negative beliefs onto themselves. This ‘self-stigma’ results from the internalisation of negative stereotypes and low self-esteem. According to research published in World Psychiatry, public and self-mental health stigma can be broken down into three components: stereotype, prejudice and discrimination.
So shaking off mental illness stigma means not only eradicating public stigma, but self-stigma too.
Myths, misconceptions & misunderstandings
One way to ensure self-stigma doesn’t stop people with mental illnesses from seeking care is to shift public perceptions. If there is more mental health awareness in society and people feel supported, then they will get the help they need. It shouldn’t matter whether it’s because they have symptoms synonymous with depression, anxiety, eating disorders, bipolar disorder, or a myriad of other mental health conditions.
Below are 5 common myths, misconceptions and misunderstandings that have cultivated the negative stereotypes associated with mental health. We need to educate ourselves and understand these myths if we want to be part of the change.
Myth #1: “There’s nothing wrong with you. It’s all in your head.”
As discussed above, when it comes to physical trauma and illness, we’re more accepting because we can see the physical signs and symptoms. But when someone has a mental illness and summons the courage to talk to us, we’re quick to dismiss this as “It’s all in your head” or, “There’s nothing wrong with you.” This could not be further from the truth. Mental illness is real, the struggle is real.
This ignorance is further compounded by the fact that in many developing countries and Eastern cultures, including the Indian subcontinent, mental illness is not recognised as an illness. In some cultures, the term ”mental health’ is a foreign concept and ‘mental illness’ is a made-up illness. Being the multicultural country that we are, it’s not uncommon to encounter such cultural perceptions and barriers to care in Australia too. Education and building awareness are critical to shifting these perceptions.
Mental illness is not a figment of someone’s imagination, nor is it a sign of weakness. According to WHO, approximately 3,000 people die of suicide daily globally and it’s the second leading cause of death in 15-29 year olds. By accepting that mental illness is a real illness we will also help eliminate self-stigma borne from this dangerous thought process.
Myth #2: You can’t help people with mental illness
Just like any physical injury or illness, people with mental illness can benefit greatly from support, love, guidance and treatment. According to the Department of Health, when treated appropriately and early, many people make a full recovery. Others may find that their condition recurs throughout life and involves ongoing treatment. This is no different to how we approach chronic physical health conditions like diabetes or asthma. It shouldn’t be a deterrent to helping someone with mental illness, nor should it feed our prejudice.
As a result of myths like this, many people don’t acknowledge they need care, or that it may help. In Australia, of the one in five adults who develop a mental illness only 35% seek care from mental health practitioners like psychologists.
Friends and family are critical components in an affected person’s life. Some ways you can help a friend or family member dealing with a mental illness are:
- Reach out to them and let them know you’re here for them.
- Ask them how they are and check in with them regularly.
- Listen to them without judgment or defining them by their diagnosis or symptoms.
- Treat them with respect and share mental health facts if you hear anything that sounds like self-stigma.
- Encourage and support them to seek care from qualified practitioners like psychologists, psychotherapists and counsellors.

Myth #3: People with mental illness are loners & unemployable
While some mental illness symptoms result in withdrawal from society, sometimes people isolate themselves because of myths like this. Public stigma around mental health conditions means that employers are often unwilling to employ people with mental illness. This also gives rise to self-prejudice which prohibits people from applying. People might also choose not to disclose their condition because they fear being discriminated against because of their mental health. This further adds to the stress and struggle they go through.
The truth is, that people with mental illness can function well in workplaces and lead productive lives. They enjoy the company of their colleagues and don’t display higher rates of absenteeism when compared to people with chronic physical conditions. In fact, with one in five Aussies reported to have a mental illness, chances are many of your work colleagues have a mental disorder. You haven’t noticed because it doesn’t impact their social skills or work.
According to the Canadian Mental Health Association, when people experience chronic mental illnesses, they learn how to manage their symptoms so they can complete their goals like working, volunteering and contributing to their community. Additionally, studies have shown that people with mental illness have average or above-average intelligence. So mental illness does not affect their competency or ability to do the job.
Myth #4: People with mental illness are violent & dangerous
The media, movies and television shows sensationalise the behaviour of mentally ill patients, particularly those with very extreme, chronic diagnoses. This highly stigmatised portrayal has fuelled the myth that people with mental illness are violent and dangerous. This misconception means that people with all forms of mental illness – be it depression, autism, or addictions to name a few – are branded negatively.
In reality, however, most people with mental illness are not violent. Violent behaviour often stems from a history of violence and criminality, not from mental illness. It’s important to correct misleading information like this because it fosters intolerance, which in turn breeds fear to seek care. This fear often stems from being labelled or even ostracised. It’s also worth understanding that people affected by mental illness are 10 times more likely to be victims of violence than the perpetrators.
Myth #5: People with mental illness are born with it
Some people may indeed inherit a predisposition to some mental illnesses like bipolar disorder and schizophrenia. While this means they have a greater chance of developing these disorders, it doesn’t mean they definitely will. Additionally, a family history of mental illness doesn’t necessarily mean you will be diagnosed with one too. Anyone can be diagnosed with a mental health disorder!
According to the Mayo Clinic, mental health disorders may be caused by several genetic and environmental factors such as:
- Inherited traits – certain genes may increase your risk of developing a mental illness and your life situation may trigger it
- Environmental exposures before birth – environmental stressors, inflammatory conditions, toxins, alcohol and drugs can sometimes be linked to mental illness
- Brain chemistry – When the neural networks are impaired, the function of nerve receptors and nerve systems change, leading to depression
The South Australian government also notes that many factors contribute to the onset of mental illness. These include stress, bereavement, relationships ending or deteriorating, social isolation, unemployment, and more.